LESSON 10 SCENE SIZE-UP AND PRIMARY ASSESSMENT. - ppt video online download

Introduction Patient assessment involves critical EMR skills Act quickly to ensure scene is safe, assess patient and care for immediate threats to life Care provided is based on patient assessment Assessment begins with the primary assessment
LESSON 10 SCENE SIZE-UP AND PRIMARY ASSESSMENT.
Act quickly to ensure scene is safe, assess patient and care for immediate threats to life. Care provided is based on patient assessment. Assessment begins with the primary assessment.
Dispatcher’s information may alert you to hazards or special precautions. Begin scene size-up before you exit your vehicle and while approaching the patient.
While approaching patient.
Hazardous Materials Chemicals Biological agents
Risk of fire or explosion. Unstable vehicles. Extrication hazards. Hazardous materials.
Potentially violent patient or bystanders. Guard dogs, wild animals.
Unstable surfaces. Water, ice. Weather extremes.
Low-oxygen areas. Toxic substances, fumes. Risk of collapse. Risk of fire or explosion.
Enter scene only if it is safe. If unsafe, make it safe or stay away and request specialized resources. Protect bystanders and other rescuers from hazards. Protect patient from environmental threats.
Address hazards within the scene. Consider the need for additional resources. Implement standard precautions to prevent infection.
Dispatch may tell you whether there is a trauma patient or a medical patient. This focuses your attention on a mechanism of injury or the nature of the illness.
MOI may suggest serious injury or presence of internal injuries.
What specifically caused the injury Was there an impact with a blunt or sharp object What body area received the impact What organs may be injured How much force may have been involved Might the force have been transferred from one body area to another
Vehicle collision may cause head or spinal injuries. Fall from a height may cause extremity fractures. Blunt impact to abdomen may cause closed injury and internal bleeding. Diving incident may cause spinal injury. Gunshot may cause extensive internal damage not apparent from the appearance of the outside wound. Fall forward onto a hand may transfer force up arm and cause shoulder dislocation.
Do not delay patient assessment to examine scene in detail. Consider MOI more fully while gathering history and performing physical examination.
Consider nature of illness during scene size-up. Don’t stop to talk to family or bystanders until you are sure there is no immediate threat to life. Observe patient’s position and demeanor for clues. Use all your senses. If patient is unresponsive, move immediately to primary assessment. If patient is responsive, ask patient, family members or bystanders why EMS was called.
Observe for clues and ask those present if everyone is accounted for. Be certain you know how many patients are involved. Call for additional help immediately for multiple patients. If more patients than responders, triage patients first.
Protect yourself and other responders. Protect the patient. Protect bystanders.
If resources not already en route, call dispatch immediately. Describe injuries in detail, so an ALS ambulance can be sent if needed.
Consider these factors: Number of patients and types and seriousness of injuries. Possible need for air transport. Potential for fire or explosion. Potential presence of hazardous materials. Need for extrication. Need for law enforcement or traffic control. Damage to power lines or other utilities.
Observe scene and patient to determine whether to use other personal protective equipment: Protective eyewear. Gown and mask. Turn-out gear. Follow standard precautions.
Rapid means to determine patient’s general condition and set initial priorities for care. Begin with your initial impression of patient. Check patient’s responsiveness, airway, breathing and circulation status. Perform primary assessment of all patients after scene size-up. If scene is safe, perform primary assessment before moving patient.
Does patient’s appearance give clues about his or her condition Are there signs of a serious problem Note patient’s sex and approximate age.
Responsive means a person is conscious and awake.
Patients who cannot talk may be able to move and thereby signal responsiveness.
Patients who cannot talk or move may be paralyzed but still able to respond with purposeful eye movements or other signs.
Begin by speaking to the patient; ask the patient what is wrong. If patient isn’t speaking or moving, tap gently and shout, Are you OK Be careful not to move patient in any way. Always suspect a spinal injury and take steps to stabilize head and neck.
Continue the primary assessment. Unresponsiveness is considered life-threatening emergency. In an unresponsive patient lying on the back, the tongue may block the airway.
Assessed with AVPU scale. AVPU scale useful for noting changes in a patient’s responsiveness while providing care and for communicating this information. Make mental note of level of responsiveness or write it down along with time. A change in level of responsiveness generally indicates a serious condition.
AVPU Scale. A = Alert. V = Responds to Verbal stimuli. P = Responds to Pain. U = Unresponsive to all stimuli.
Responsiveness in pediatric patients. Infants and young children may respond differently from older children and adults. Look for age-appropriate responses. Assess unresponsive infant by flicking bottom of feet and noting response.
A patient who can speak, cough or make other sounds is breathing and has a heartbeat. Reflex gasping (agonal respirations) may be present just after cardiac arrest; do not confuse this with normal breathing. Lack of breathing may be caused by cardiac arrest, obstructed airway or other causes. If patient is not breathing normally, quickly move to next step and check for a pulse.
If patient’s heart has stopped or patient is bleeding profusely, vital organs are not receiving enough oxygen to sustain life. Do not use more than 10 seconds to feel for the pulse unless a pulse is clearly found in that time, start CPR. If the patient is responsive or breathing, the heart is beating.
Note rate, rhythm and strength.
In an unresponsive adult, check carotid pulse (no longer than 10 seconds)
In an unresponsive child, check either carotid pulse or femoral pulse. In an infant, use the brachial pulse in the inside of the upper arm.
Do not take time to count pulse, note whether it is irregular, very slow or very fast signs that patient may not be stable. Lack of pulse along with absence of normal breathing signifies heart has stopped or is not beating effectively enough to circulate blood. If patient lacks a pulse and is not breathing normally, start CPR and call for an AED.
Inadequate breathing is characterized by diminished mental status and any of these: Difficult or labored breathing. Wheezing or gurgling sounds with breathing. Pale skin (ashen skin in a dark-skinned patient) or a blue (cyanotic) color of the lips and nail beds. A respiratory rate in an adult slower than 10 or greater than 30 breaths a minute. Give emergency care for a patient with a pulse who is breathing inadequately.
Look for life-threatening bleeding. Arterial bleeding usually most serious. Bleeding from vein is generally slower.
Don’t remove clothing to check for bleeding, but look for blood-saturated clothing and blood pooling. During primary assessment, don’t address minor bleeding or wounds. Control serious bleeding immediately with direct pressure.
Even with a pulse, circulation may be inadequate. Inadequate oxygenation of vital organs results in life-threatening shock.
Heart rate in an adult <60 or >100. Irregular pulse may be normal or abnormal. Pale skin may indicate blood loss, shock or low body temperature. Bluish skin may indicate an airway problem, poor ventilation or respiration, or poor blood flow. Cool skin temperature may indicate low body temperature or shock. Sweaty or wet skin may indicate shock, severe pain or physical exertion. Slow capillary refill (>2 seconds) in children may indicate shock.
If patient is unresponsive to verbal stimulus, has a fast or slow heart rate, and has skin signs of shock, treat for shock after the primary assessment. If patient has any life-threatening condition, treat it as soon as it is discovered. If patient has no immediate threat to life, proceed to secondary assessment.
Check for responsiveness and normal breathing. If patient is unresponsive, call for more EMS resources. If unresponsive patient is not breathing normally, also call for an AED. If patient is not breathing, check for a pulse for no longer than 10 seconds. If no pulse, start CPR. If a pulse, start ventilations. If patient is breathing, check for severe bleeding, shock and other threats to life. Care for any life-threatening conditions before continuing to check the patient and provide other care.
Unresponsiveness or any problem with the airway, breathing or circulation is a high priority. Continue to reassess and treat life-threatening conditions while waiting for additional EMS resources. Call EMS unit to update patient’s condition.
Provide this information: Number of patients. Patient age and gender. Patient’s condition. Patient’s level of responsiveness. Patient’s breathing and circulation status. Ask responding unit their estimated time of arrival. Continue to care for patient accordingly. With stable patient, proceed to secondary assessment.
PPT - SCENE SIZE-UP AND PRIMARY ASSESSMENT PowerPoint Presentation, free download - ID:4941286

EMERGENCY MEDICAL RESPONDER LESSON 10: SCENE SIZE-UP AND PRIMARY ASSESSMENT
PPT - Scene Size-up PowerPoint Presentation, free download - ID:1710228
LESSON 10 SCENE SIZE-UP AND PRIMARY ASSESSMENT. - ppt video online download

LESSON 10 SCENE SIZE-UP AND PRIMARY ASSESSMENT. - ppt video online download
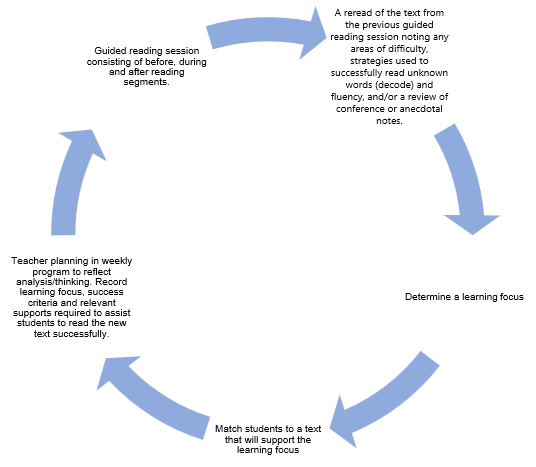
Guided reading

Steps to Primary Assessment (Initial Assessment) after Scene Size-Up
Scene size up and initial assessment

Scene Size up and primary assessment